Making how tell someone a little easier.
Sharing what’s bothering you
Sharing what’s bothering you can help to make it feel more manageable. If you feel that the problems you’re having are too big for you to deal with by yourself you may want to get in contact with your GP, someone from school/college or someone else you trust.
- Childline can help with support including distractions and access to a coping kit.
- Doc Ready can assist you to start a conversation with your GP about mental health.
- ChildLine have produced a short video about depression for young people.
- Thinkuknow is a guide to internet safety For all ages, parents and professionals.
Know your rights about confidentiality
Confidentiality means not telling anyone the things you’ve told them or they’ve told you. It means you can trust that they will keep it private.
Telling someone about self-harm is hard, and whoever you tell should respect your right to privacy. However, there are times when they may have to let other people know if they are really worried about your or someone else’s safety.
If you talk to someone who you know through their professional role, they’ll need to ensure you get the support you need to help you to get on top of things. They’ll tell you that they can’t keep confidentiality. Breaking a young person’s confidentiality is not something people do unless they have to. And they should always try to talk to you about it first if they can.
You can talk to them about who needs to know what – but try to remember it’s a good thing that people understand what’s going on so they can help you, though it might seem a bit scary at first.
There’s no reason for you to deal with things all on your own; if you’re really worried about talking to someone face-to-face, you can call, email, or even text a professional support group or helpline anonymously and confidentially. See the end of this page for organisations that can help.
Think about what you want to happen next
It’s a big step to ask for help and it usually means that on some level you’re ready for things to improve. Do you have any idea of what you might like to happen as a result of the conversation you’re planning? This might include:
- Support to tell your parents or a friend
- First aid or medical help for injuries
- Support to help you talk through and overcome underlying issues
- Referral for specific treatment that you’re already aware of
- You’re not sure, you just can’t carry on with how things are
Even if you’ve gone looking for help, it can be hard to accept it – but try. Have faith in the person you’ve confided in to help you to take the first steps to make things better. They won’t be able to fix everything all in one go, but they can work with you to start to make things change.
Who can I talk to about self-harm?
Telling anyone about your self-harm is a massive and brave step, perhaps ask a friend to be with you? Talking to a trained health professional such as your doctor (GP), a counsellor or support organisation is a safe move because they should listen calmly and offer you objective advice. It might also be easier to open up to someone you’re not emotionally close to because you can relax and not worry about upsetting them.
What does confidentiality actually mean when it comes to self-harm?
Different people have different rules of confidentiality if you open up to them about self-harm. We talk you through the confidentiality guidelines of the main people you may turn to.
What if I’m under 18?
If you’re aged 16 or 17, the law sees you as an adult when it comes to confidentiality and consent to treatment. Therefore, if you’re 16 and you want a health professional to keep your treatment confidential then that should be respected.
Will my doctor tell anyone I’m self-harming?
In most cases, no. All staff working for the NHS have a legal duty to follow the NHS Code of Practice on Confidentiality. This means they must ask for your consent before passing information to anyone else – this is part of their duty of care and applies whatever age you are.
When will a doctor tell anyone I’m self-harming?
In most cases, never. However, there are exceptions to this rule This is normally when they feel you don’t have ‘mental capacity’, i.e. when you may not be able to make certain decisions because they feel you won’t understand the advice, or your physical or mental health is likely to suffer unless you receive treatment or support.
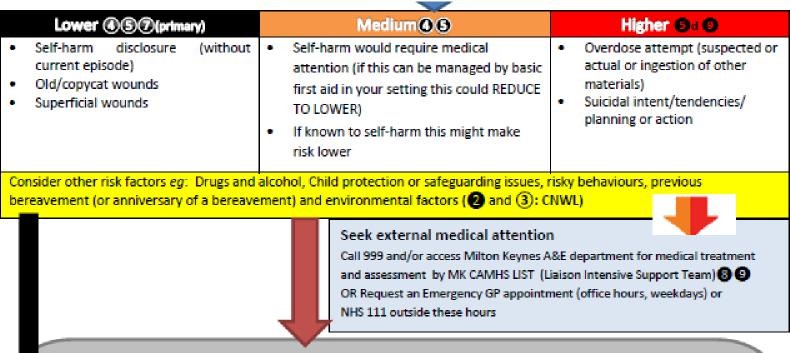
This also applies where there are issues around child protection; when they are worried you may harm yourself more seriously than you meant to; if you’re expressing suicidal feelings; you’re being sexually or physically abused; or your self-harm will lead to permanent damage.
If they do decide to contact someone else, then they should let you know they are going to do that first.
Can a doctor or a therapist tell my parents I’m self-harming?
Parents don’t have an automatic right to know what is said during your treatment with a mental health professional, even if you’re under 16 and if they’ve given permission for you to have the treatment in the first place.
There are some exceptional circumstances when a doctor can disclose information about you without your consent, even if you have mental capacity and are considered ‘competent’. An example of this is if the doctor is concerned that you are going to kill yourself – it wouldn’t necessarily be that they would tell your parents (if they do they must tell you they will do this), but they may talk to another professional such as psychiatrist or social worker.
Will my parents or doctor be told if I go to A&E for self-harm?
If you’ve been to an emergency department because you’ve self-harmed, a very brief letter will go to your GP which states why you came in and what investigations you had. There is a confidentiality policy, but this doesn’t exclude doctors talking to each other where it’s helpful they know about self-harm. If you really object to this then it’s down to the health
professional to decide if this should be respected.
What if I tell a teacher I’m self-harming? Will they tell someone?
Teachers have a legal duty not to keep certain things to themselves. If you confide in a teacher, they should refer you to an experienced counsellor or health professional who knows how best to help and support you. “We can’t keep anything confidential in terms of self-harming or abuse, and we do have to refer it,” says Jo, a secondary school teacher. “But it won’t necessarily be to your parents, but within the school, such as the school’s designated Child Protection officer, the school nurse, or the head teacher.”
How do I get help from CAMHS?
( Milton Keynes Specialist Child and Adolescent Mental Health Service - CAMHS)
Someone, usually your parents, teacher, GP, or yourself if old enough, can refer you for an assessment with CAMHS to see what help you could get.
If you're being supported by social care, a youth offending team or a service at your school, they might also be able to refer you.
It's important to tell the person referring you as much as you can so you can get the help you need.
How do I get in touch with CAHMS?
CAMHS in Milton Keynes have a website where you can look up how to get access to their service.
Supporting others - I'm worried about a friend
If one of your friends or group is in trouble, upset or showing signs of self-harming it’s important that you feel supported to help them. Friends can worry about betraying confidences so you need to know that self-harm can be very dangerous and that by seeking help and advice for a friend you are taking responsible action and being a good friend. You should also be aware that your friend will be treated in a caring and supportive manner.
Friends and family can play a huge role in helping people get the support they need – it’s not always down to them to do it.
Two thirds of young people with a mental health problem say that fear of judgement has stopped them telling a friend. Getting support from parents, teachers and professionals is important, but having a mate in their corner can make a big difference too. If you’re open about mental health, you can show your friend that it’s ok to be open and talk about mental health problems.
My Friend is Self-Harming – How can I help them?
- You can really help by just being there, listening and giving them support when they need it
- Be open and honest. If you are worried about your friend’s safety, you should tell an adult. Let your friend know that you are going to do this and you are doing it because you care about them
- Encourage your friend to get help, for example from their GP. You can go with them for support
- Your friendship may change. You may feel bad that you can’t help your friend enough or guilty if you tell an adult. These feelings are common and doesn’t mean that you have done something wrong
Tips:
Just being there for your friend can make a big difference, and you don’t have to be an expert to help your friend
If you’re worried about a friend, consider telling an adult – someone who can be there for you, and happy to talk about things and support you if it becomes too much.
You could do some research online (e.g. Young Minds or Childline) and find out more about the condition that your friend is experiencing – this will help you to build confidence talking with them.
There are a few things you can do to help:
- Offer to listen
- Keep an open mind
- Help them to manage their problems
- Offer to go with them to get help
- Don’t treat them any differently from normal
- Be prepared and ask someone to support you too:
- It can be difficult to look after someone who is having difficulties. It is important for you to find an adult to talk to, who can support you. If you’re finding it hard to talk to other people contact Childline for some advice.
- You may not always be able to be there for your friend and that's OK.
- Your friendship may be changed by the problem. You may feel bad that you can't help your friend enough or guilty if you have had to tell other people. These feelings are common and don't mean that you have done something wrong/not done enough.
- Your friend may get angry with you or say you don't understand. It is important to try not to take this personally. Often when people are feeling bad about themselves they get angry with the people they are closest to.
Remember, you don’t need to understand why they self-harm. The key is simply to listen, help them find the support they need and most importantly, don’t make them feel ashamed or embarrassed by it.
- You can really help by just being there, listening and giving support.
- Be open and honest. If you are worried about your friend's safety, you should tell an adult. Let your friend know that you are going to do this and you are doing it because you care about him/her.
- Get information from telephone helplines, websites, the library etc. This can help you understand what your friend is experiencing.
- Encourage your friend to get help. Explain that by sharing what’s bothering them can help to make it feel more manageable.
- You can go with them or tell someone they want to know.
Thinking about what might support you in school (Safety Plan)
If the school knows about your self-harm they will work with you to understand how they and others can support you. One of the things that might be suggested is a support plan (also called a ‘Safety Plan’). It is essential that the plan is created together with you as it details how YOU want to stay safe. The plan must be something that you feel you are able to agree to. If you haven’t told anyone in school, you can still use this as a way to support yourself to be safe in and out of school.
Making your support plan
You may want to consider the following statements or questions and answer them, perhaps with help, so that you can agree how you can be supported in school, at all times, but particularly when you are finding things difficult.
- I might feel like self-harming if...
- My warning signs are...
- Who or what can distract me?
- I can... (Distractions, coping strategies, what takes my mind off things?)
- If I need a safe place I can go to...
- I will tell myself that... (positive affirmations)
- Who can I ask for help?
- How will I show or tell them I need help?
- I’d like people to help me by ...
- I can also access support from (agencies, apps, websites, text messaging) I agree this plan can be shared with...
Taking care of myself – tips and hints for good mental health
Sometimes it seems like we have little or no control over what we think and how we feel. But, there are things that you can do that will help you to feel better.
Diet
Food can affect your mood! There is a link between what we eat and how we feel so it’s important to have a healthy, balanced diet for both your body and mind.
Exercise
Everyone knows that exercise is good for your body – but it’s also important for your emotional wellbeing. Scientists have discovered that exercise causes your brain to release chemicals that make you feel good. There is evidence to show that exercise can help raise self-esteem, help sleep problems, improve memory and concentration, takes your mind off negative thoughts, as well as reduces feelings of anxiety and depression.
Improving your self-esteem
Self-esteem is how you think and feel about yourself. Having healthy self-esteem makes it easier to cope with life’s ups and downs. If you have low self-esteem, the thoughts and feelings you have about yourself tend to be negative. This can make you more prone to mental health problems.
Taking time to relax
Regular relaxation is beneficial for your mental health. If you make a regular time each day to practice some of the techniques below you will get better and better at relaxation and notice your day-to-day stress levels are lower. You will also become able to use relaxation at the times you need them most.
Improve relaxation, reduce stress and anxiety by changing the way that you breath:
Another great way to relax is to practice mindfulness. This is the focusing of attention and awareness on the here and now, and is often used to reduce anxiety, stress and depression. It has its roots in Buddhism, though is used widely by people of all ages from all different backgrounds with all sorts of problems.
- About mindfulness information from Mind that might help you relax and improve your sense of wellbeing.
Source: With thanks to CNWL CAMHS website .
Compiled in conjunction with the Self-Harm Toolkit Working Group and Public Health, Milton Keynes City Council.
This version (V4) refreshed May2025.
This document is not comprehensive and new on-line resources and apps are being developed all the time. If you know of anything that you think we should include in this list or deleted, please pass on the details to us at: public.health@milton-keynes.gov.uk.